Written by Michelle Terhune
We want to help you make educated healthcare decisions. While this post may have links to lead generation forms, this won’t influence our writing. We adhere to strict editorial standards to provide the most accurate and unbiased information.

If someone you know is one of the more than 3.5 million Americans living with autism spectrum disorder (ASD), you may want to learn more about this condition and also find out how you can help.
The first thing to know is that while there’s no cure for autism, the condition is treatable. Multiple studies have found that early diagnosis and treatment in children decreases their symptoms and improves their skills. In fact, a few children actually move off “the spectrum” (as it’s often called) as they get older.
But to get more kids diagnosed sooner, it’s important to continue building awareness about autism. World Autism Awareness Day, which recognizes the rights of those on the autism spectrum, is celebrated every year on April 2.
Is There Insurance Coverage for Autism Treatment?
ASD is expensive to treat; children and teenagers with autism have medical expenses four to six times higher than young people without ASD. Behavioral therapies for children with autism, for example, cost $40,000 to $60,000 annually, on average.
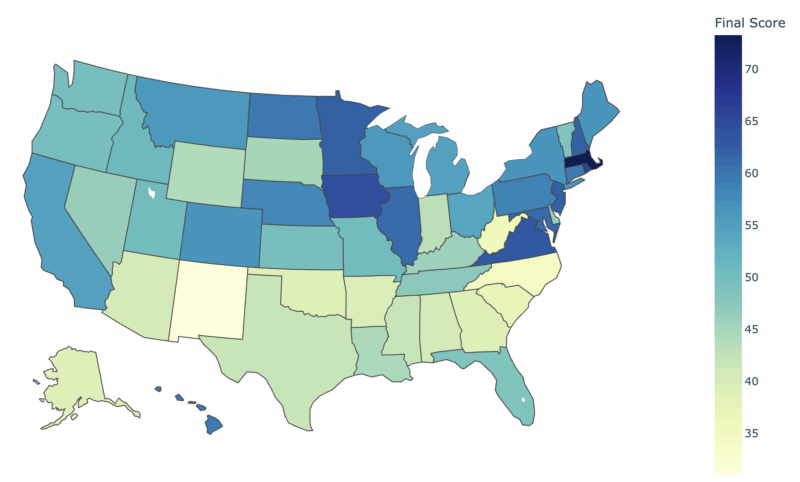
Fortunately, 46 states and the District of Columbia have passed laws requiring some sort of health insurance coverage for autism. Some states require plans to provide the same benefits for autism as for any physical illness. Some specify maximum annual benefit amounts, cap lifetime limits or require age-based coverages. Other states also address autism through their Medicaid programs, taking advantage of autism-specific Home & Community-Based Services (HCBS) waivers.
Autism is considered a preexisting condition, so if you get your health insurance through federal or state Health Insurance Marketplace insurers, you can’t be denied coverage. That’s because the Affordable Care Act (also known as Obamacare) doesn’t allow denials of coverage for anyone with a preexisting condition. If you buy a Marketplace plan, you’ll also get coverage for free autism screenings for children.
Families whose insurance plans don’t cover all the costs of autism treatment may be able to deduct the expense on their itemized income tax return.
How Prevalent is Autism in the U.S.?
The Centers for Disease Control (CDC) tracks how common autism is in the U.S. and how these numbers have changed over time. Prevalence is the number of people with a condition among a certain group or population. The CDC estimates that one in every 54 eight-year-olds in the U.S. has been diagnosed with autism. Here’s what else you should know about the prevalence of autism in the U.S.:
It has increased over time.
No one can say for sure whether the increase is because more kids are developing ASD or because experts are doing a better job of screening and diagnosing autism. Since starting treatment earlier is critical to a child’s progress over time, this is a positive trend.
Prevalence isn’t the same across the country.
Some states have fewer than 10 children with ASD for every 1,000 residents, while others have 30 kids or more. Although no studies show a link between geography and having autism, these variations might indicate that some communities are more aggressive in screening and diagnosing the condition or have more effective methods of collecting that information.
There’s a difference between girls and boys.
Since 2000, prevalence rates for boys have been higher than for girls. The reason is unknown, but boys might be at greater risk of developing autism, or they may show different signs and symptoms than girls do.
Prevalence also varies by race and ethnicity.
Data from 2016 shows no difference in prevalence between non-Hispanic white children and non-Hispanic Black children. But rates of ASD among Hispanic children were lower, although there wasn’t as big a difference as in previous years. It could be that stigma about being diagnosed with autism, lack of access to healthcare and language issues have meant a lower rate among Hispanic kids. The closing of the gap could indicate these barriers are diminishing as outreach to the Hispanic community improves.
2020 Community Report from CDC Satellite Study
The CDC recently released its biennial Community Report on Autism, based on data collected in 11 states (Arizona, Arkansas, Colorado, Georgia, Maryland, Minnesota, Missouri, New Jersey, North Carolina, Tennessee, Wisconsin).
The CDC aims to obtain data that establishes the prevalence of autism in communities, including by race and ethnicity; intellectual disability (such as lower IQ); age of diagnosis; and community impact over time. This data will help ensure early identification and diagnosis of all children with autism with the hope that this information will guide public policy and research.
How Can You Promote Autism Awareness?
Raising awareness is key to early diagnosis and intervention among children with autism spectrum disorder. Here are three ways you can help.
Donate, If You Can.
Consider giving to any of these four organizations:
Autism Research Institute was founded on the belief that autism is treatable. It seeks to support those affected by ASD through innovative, impactful research and education. The organization funds research grants connects scientists with clinicians and recruits participants for ongoing autism research.
Autism Society of America is an advocacy, education, referral and support organization with a nationwide network of affiliates. Its Autism Source database is a comprehensive, searchable source of information on everything from physicians and therapists,education and government services, parent resources, and more.
Autism Speaks aims to improve the lives of those with autism, and that of their families, throughout their lives through advocacy, increased awareness of and acceptance of those with the condition and by being a catalyst for autism research. Autism Speaks influences federal and state public policy.
Organization for Autism Research (OAR) was founded by seven people whose lives and families were affected by autism. OAR is a parent-led, science-based and community-focused organization dedicated to funding research and applying lessons learned to improve the outcome and the lives of those diagnosed with autism.
2. Learn More About Autism.
The Autism Society offers resources you can use to educate yourself about the condition:
Next Steps: A Guide for Families New to Autism is an eight-page guide for families of those recently diagnosed with autism. It provides an overview of the spectrum, treatment options and the education, services and support available to children and adults with autism and their families.
Building Our Future: Educating Students on the Autism Spectrum is a 12-page guide for teachers working with students who are on the spectrum. Educators and administrators are more effective when they understand the learning styles of students with ASD and methods designed to meet their unique needs.
For a full list of resources, visit the Autism Society’s “Living With Autism” series designed for individuals on the autism spectrum and their families, friends and concerned professionals.
Stimming, Hand Flapping and Other Self Stimulatory Behaviors in Autism is a guide discussing everything you need to know about stimming in children with ASD and how to manage stimming behaviors.
Planning Across The Spectrum, Special Needs Event Calendar. Sign up for a newsletter of events.
3. Put Social Media to Use.
Hashtags are a great way to promote awareness and make information about autism go viral. They not only raise general awareness but drive people affected by autism to valuable resources. Here are some of the hashtags you can use in your social media posts on Facebook, Twitter, Instagram, Tumblr, LinkedIn, Google+, and Pinterest:
#autismawareness #autism #autismacceptance #autismmom #autismfamily #asd #specialneeds #autismspeaks #autismlife #autismlove #autistic #autismsupport #autismspectrum #autismo #autismspectrumdisorder #aspergers #autismparents #actuallyautistic #autismdad #differentnotless #autismadvocate #autismawarenessmonth #sensoryprocessingdisorder #neurodiversity #autismparent #worldautism #specialneeds #autismjourney #autismcommunity #autismworld #autismrocks #neurodivergent
Specific State Insurance Laws
| U.S. State | Statue Summary | Full State Details |
| Alabama | Requires coverage for screening, diagnosis and treatment for insured children age nine and younger by employers with 51 employees or more. Coverage may not be subject to dollar limits, deductibles or coinsurance less favorable than other illness, except for behavioral therapy which is subject to $36,000 annual limits. | Alabama Act No. 2012-298 |
| Alaska | Generally requires coverage for diagnosis and treatment for insureds age 21 and younger by employers with more than 20 employees. Coverage is not subject to limits, deductibles or coinsurance less favorable than other illnesses. | Alaska Sec. 21.42.397 |
| Arizona | Requires some insurers to cover diagnosis and treatment with no difference in limits, deductibles or coinsurance than other covered illnesses. Behavioral therapy may not be excluded but subject to $50,000 annual limit for children up to age 9 and $25,000 limit for ages 9-16. | Arizona Revised Statute 20-826.04 and 20-1404.03 |
| Arkansas | Requires coverage for diagnosis and treatment with an annual limit for behavioral therapy of $50,000 for children under age 18. There are no limits on the number of provider visits. Coverage exceeding requirements for ACA plans is not required of insurers offering plans through the state medical exchange. | Arkansas 2011 Act 196 (HB 1315). |
| California | Requires coverage by disability insurance, health insurance and healthcare service plans for diagnosis and treatment, including behavioral therapy. Coverage not required to exceed benefits required for ACA plans. | California Insurance Codes 10144.5, 10144.51 and 10144.52. Health and Safety Codes 1374.72 and 1374.73 |
| Colorado | Requires health plans to include coverage for assessment, diagnosis and treatment with behavioral therapy limits of $34,000 for children under age 9 and $12,000 for children age 9-18. | Colorado SB 09-244 |
| Connecticut | Requires group health plan coverage for diagnosis and treatment, and group and individual plan coverage for physical, speech and occupational therapies. Behavioral therapy limits are $50,000 for children under age 9, $35,000 for ages 9-12 and $25,000 for ages 13-14. | Connecticut Public Acts 09-115, 11-4 and 08-132 |
| Delaware | Coverage required for assessment, diagnosis and treatment for those under age 21. Annual coverage limits for applied behavioral analysis in various age groups. Coverage may be no less favorable than for any physical illness. Insurers have the right to request review of treatment. | Delaware Statute 3361 |
| District of Columbia | Requires coverage for habilitative services, defined as occupational, physical and speech therapy, for children under age 21. Coverage should be no less restrictive than for any illness, condition or disorder. Plans are not required to reimburse for services delivered through early intervention or schools. | DC Code 31-3271 and 31-3272 |
| Florida | Requires health plans and maintenance contracts to cover well-baby and well-child screenings, and treatment through speech, occupational and physical therapies and applied behavioral analysis. Coverage for treatment prescribed by treating physician up to $36,000 annually with $200,000 lifetime benefit limits. | Florida Statute 627-6686 and 641.31098 |
| Georgia | Requires coverage for screening, diagnostic testing and treatment. Coverage required by group and individual health plans as with any neurologic disorder | Georgia Code 33-24-59.10 |
| Hawaii | Requires coverage for screening, diagnosis and evidence-based treatment for all insureds under the age of 21. Maximum annual benefit of $50,000 and lifetime cap of $300,000. ABA cap $25,000 per year up to age 14. | Hawaii Senate Bill 791 |
| Idaho | Requires individual and group insurance plans to cover evidence-based treatment, including applied behavioral analysis. | Idaho Department of Insurance Bulletin No. 18-02 |
| Illinois | Requires coverage by individual and group accident, health insurance and managed care plans for diagnosis and treatment for those under age 21. Also requires coverage of habilitative services for those under age 19. Required coverage for applied behavioral analysis is limited to $36,000 per year. | Illinois Revised Statute 215 5/356z.14 and Public Act 095-1049 |
| Indiana | Requires individual and group accident and sickness insurance policies and health maintenance contracts to cover treatment as prescribed by physician’s treatment plan. Insurers cannot refuse, deny or otherwise restrict coverage for anyone diagnosed with ASD. | Indiana Code 27-8-14.2-1 and 27-13-7-14.7 |
| Iowa | Requires certain health plans to cover treatment. Requires all state employee plans to cover diagnosis and treatment for insureds up to age 19. Annual maximum benefit of $36,000 but prohibits limiting number of visits to healthcare providers. | Iowa Code 514C.28 and Rule 191-35.40 |
| Kansas | Requires state employee health plans, group plans, medical service plans, hospital and medical service contracts, health maintenance organizations and fraternal benefit plans to cover diagnosis and treatment, including applied behavioral analysis and evidence-based treatments for insureds up to age 19 with age-related annual caps. | Kansas Statute 75-6524 and 40-2,105a |
| Kentucky | Requires large group health plans and state employee plans to cover diagnosis and treatment from age 1 through 21. Caps of $50,000 annually for those age 1 until seventh birthday and $1,000 monthly for ages 7-21. Individual and small group plans must provide coverage for treatment up to $1,000 monthly. | Kentucky Revised Statute 304.17A-142 |
| Louisiana | Requires most group health insurance plans and health maintenance organizations to provide coverage for diagnosis and treatment for individuals up to age 21 with maximum benefit capped at $36,000. | Louisiana Revised Statute 22:1050 |
| Maine | Requires individual and group health plans and health maintenance organization contracts to cover diagnosis and treatment for insureds age 5 and under. Annual coverage for applied behavioral analysis may be capped at $36,000 but number of visits may not be limited. Coverage may be no less restrictive than for physical illnesses. Reimbursement also applied to home and community programs under the state’s Medicaid program. | Maine Statute 24-A Section 2768, Section 2749C and Section 2325 |
| Maryland | Requires health insurers and nonprofit health service plans and health maintenance organizations to cover habilitative services for insureds up to age 19. They are not required to provide reimbursement for early intervention or school services. | Maryland Insurance Code 15-835 |
| Massachusetts | Requires certain individual, group and state employee health plans and health management contracts to cover diagnosis and treatment and may not assert annual or lifetime limits less than for any other illness. Also may not limit number of annual provider visits. | Massachusetts General Law 32A-25 and 32A-22 |
| Michigan | Requires individual and group health maintenance organization contracts to cover diagnosis and treatment. Coverage may be limited to annual benefit of $50,000 for children through age 6, $40,000 for ages 7-12 and $30,000 for ages 13-18. Plans offered through the state health exchange are not required to cover more than the ACA requires. | 2012 Michigan Public Act 100 |
| Minnesota | Requires all large group health plans and state employee insurers to cover diagnosis, evaluation and treatment for children under age 18. Children insured under the state’s medical assistance program receive intensive early intervention and treatment up to age 21. | Minnesota Law Chapter 108-H.F.No. 1233 |
| Mississippi | Requires health insurance plans to cover screening, diagnosis and treatment determined to be medically necessary by a licensed physician or psychologist. Coverage limits, deductibles and coinsurance must be no less than coverage for medical and surgical plans. | Mississippi Code 83-9 |
| Missouri | Requires all group health plans to cover diagnosis and treatment limited to that prescribed by a physician’s treatment plan. Maximum annual coverage for applied behavioral analysis is $40,000 through age 18, although that limit may be exceeded with plan approval. Plans may not limit number of provider visits. | Missouri Revised Statutes 337.300 et. seq. and 376.1224 |
| Montana | Requires specified disability policies, certificates of insurance and membership contracts to cover diagnosis and treatment for those age 18 and younger. Annual limits are $50,000 for children age 8 and younger and $20,000 for age 9 through 19. Benefits must be no less than for other physical illnesses. | Montana Code 33-22-515 |
| Nebraska | Requires individual and group health plans to cover screening, diagnosis and treatment. Behavioral therapies are limited to 25 hours per week until the insured reaches 21 years of age. No limits may be applied to the number of other provider treatments and coverage limits may not be more restrictive than those for physical illness. | Nebraska Revised Statutes 44-7,106 |
| Nevada | Requires individual and group health plans and health maintenance organizations to cover screening, diagnosis and treatment for insureds under the age of 18 or if enrolled in high school, until an insured reaches age 22. | Nevada Revised Statute 689A.0435 |
| New Hampshire | Requires specified health insurers to cover treatment and services including applied behavioral analysis. Coverage for ABA may have annual limits of $36,000 for insureds ages 0 to 12 and $27,000 for insureds ages 13-21. Coverage cannot be limited to more than policies for physical illness. | New Hampshire Revised Statute 417-E:2 and 417-E:1 |
| New Jersey | Requires specified health insurance policies and health benefits plans to cover expenses for screening and diagnosis, then for medically necessary occupational, physical and speech therapy. If the insured is under age 21, policies must cover expenses for behavioral therapies including applied behavioral analysis. | New Jersey Public Law 2009, Chapter 115 |
| New Mexico | Requires specified health plans, policies, certificates and contracts to cover screening, diagnosis and treatment for insureds age 19 and younger or age 22 and younger if enrolled in high school. Treatment includes therapies and behavioral analysis, Coverage limited to $36,000 per year and $200,000 lifetime. | New Mexico Statute 59A-22-49 and 59A-23-7.9 |
| New York | Requires specified health insurance policies and contracts that provide insurance for hospital and surgical services to not exclude coverage for screening, treatment and diagnosis. No limitations on number of provider visits. Annual limit for applied behavioral analysis is $45,000. | New York Insurance Law 3216, 3221 and 4303 |
| North Carolina | Requires coverage for screening, diagnostic testing and treatment and insurers are prohibited from terminating coverage or refuse to issue, amend or renew coverage based on the diagnosis. | North Carolina Statute 58.3.220 |
| North Dakota | Requires all individual and group health insurance plans to cover treatment, including applied behavioral analysis, as prescribed by a physician in a treatment plan. Prohibits caps and limitations on coverage for other treatment. | Senate Bill 2268 |
| Oklahoma | Requires coverage under certain circumstances and prohibits limits on provider visits. Requires coverage equal to physical issues and coverage for applied behavioral analysis. State Insurance Commissioner is allowed to adjust annual maximum limits yearly. | Oklahoma Statute 36-6060.20, 36-6060.21 and 36-6060.22 |
| Ohio | Requires insurance coverage for screening, diagnosis and treatment. Insurers are prohibited from terminating coverage or refuse to issue, amend or renew coverage based on the diagnosis. Copayments, coinsurance and deductibles must be the same as for other illnesses and procedures in the policy. | Ohio Revised Code 3923.84 |
| Oregon | Requires specified coverage by health benefit plans, Public Employees’ Benefit Board and Oregon Educators’ Benefit Board. Requires licensing of providers of applied behavioral analysis to qualify for reimbursement. | Oregon Revised Statutes Chapter 676 |
| Pennsylvania | Requires health insurance policies and government plans to cover diagnostic assessment and treatment for insureds under the age of 21. Maximum annual benefit cap is $36,000. | Pennsylvania Statute 40-764h |
| Rhode Island | Requires specified health insurance policies and contracts to cover treatment and therapies, including applied behavioral analysis, to insureds up to age 15. Annual limit for applied behavioral analysis is $32,000. | Rhode Island Statutes Chapter 27-20.11 |
| South Carolina | Requires health insurance plans to cover treatment specified by provide in a treatment plan. Coverage for insureds diagnosed at age 8 or younger and be younger than 16 years of age. | South Carolina Code of Laws Title 38 Chapter 71 |
| South Dakota | Requires coverage for applied behavioral analysis, subject to pre-authorization, prior approval and care management requirements such as limitations on number of visits, dollar limits, deductibles, copayments and coinsurance that apply to other medical and surgical limits in the policy. | South Dakota Statute 58-17-157 and 58-17-154 |
| Tennessee | Requires that health insurance policies and contracts that provide coverage for neurological disorders provide coverage for treatment for insureds under the age of 12. | Tennessee Code 56-7-2367 |
| Texas | Requires coverage of all generally recognized services for treatment prescribed by insured’s primary care physician as part of a treatment plan. The plan must provide coverage from the date of diagnosis until the insured completes 9 years of age. Coverage may be subject to the same deductibles, coinsurance and copayments as the rest of the plan. | Texas Insurance Code 1355.015 |
| Utah | Requires individual and group health insurance plans to provide coverage for treatment of children at least 2 years old and younger than 10 years old. | Utah Statute 31A-22-642 |
| Vermont | Requires coverage of evidence-based diagnosis and treatment, including applied behavioral analysis, from birth through age 21. Plans offered through state’s health benefit exchange are required only to meet the requirements of the ACA. | Vermont Statute 8-4088i and 2012 Vermont Acts 158 |
| Virginia | Requires health insurers, subscriptions and health maintenance organizations to cover treatment for insured from age 2 to age 6, unless coverage costs exceed 1% of premiums charged. Applied behavioral analysis benefits are limited to $35,000 annually unless the plan approves higher limits. There is no limit on number of provider visits. | Virginia Code 38.2-4319 and 38.2-3418.17 |
| Washington | Requires health insurers, prescription plans and health maintenance organizations to cover diagnosis and treatment. Also requires coverage through the state’s ACA exchange and Medicaid program. | Washington State Senate Bill 5059 |
| West Virginia | Requires specified insurers, including the state’s CHIP to cover diagnosis and treatment of insured from age 18 months through 18 years. Children must be diagnosed by age 8 or younger to qualify. Maximum for applied behavioral analysis is $30,000 per year for the first three years and $2,000 per month thereafter. | West Virginia Acts 2011 Chapter 13 |
| Wisconsin | Requires specified disability insurance plans and self-insured plans to cover treatment if prescribed by a physician. No insurance company may refuse, cancel or deny coverage based on an autism diagnosis. | Wisconsin Statute 632.895 |
| Wyoming | Requires health insurance with mental health coverage to include treatment for ASD. Plans that provide benefits for both medical/surgical and mental health cannot have more restrictive requirements for deductibles, copays, coinsurance and treatment limitations that for physical illnesses. | Mental Health and Substance Use Disorder Insurance Parity Act |
Next Steps
The rising prevalence of those on the autism spectrum means that more and more people will be affected in some way by children and adults living with this condition. That means families, educators, employers, co-workers and communities need a better understanding of the unique challenges faced by those with autism.
Share this information in person with family, friends and colleagues and digitally as well. And don’t forget to join the efforts surrounding World Autism Awareness Day every year on April 2.
Educate yourself. Educate others. Spread the word. Raising awareness is the first ripple of a wave.
Thank you for your feedback!