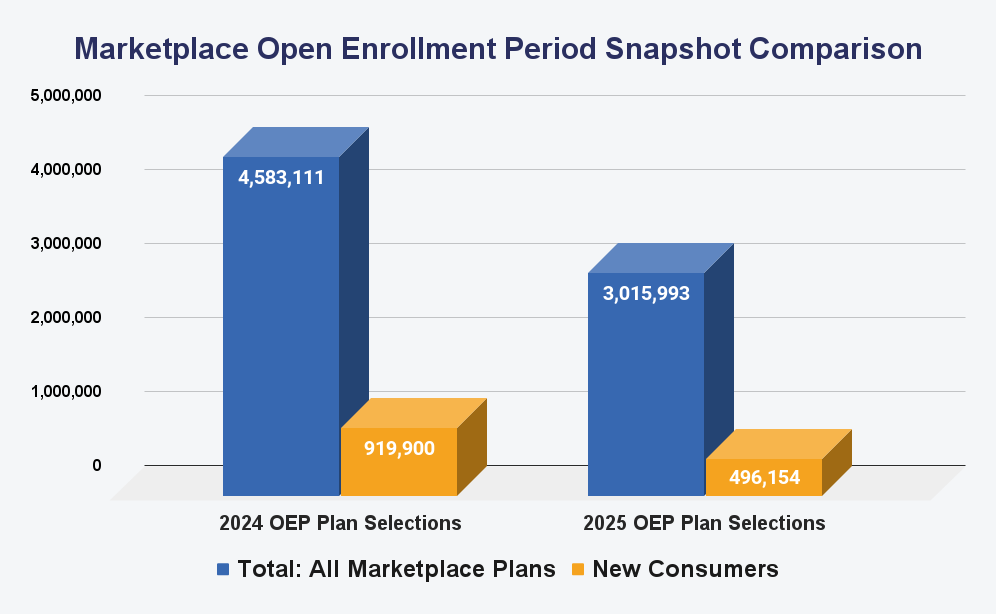
In 2024, the ACA marketplace encountered various obstacles that contributed to a 31.2% year-over-year decline in returning enrollees.
This drop can be attributed to various factors, including implementing a new three-way verification process, states like Georgia transitioning to state-based exchanges, and the distractions associated with an election-year impact.
Additional complexities arose from the Special Enrollment Period (SEP) for those losing Medicaid coverage, discrepancies in data, and ongoing concerns about the accuracy of last year’s enrollment figures.
One of the most significant changes was the introduction of a three-way verification process in July 2024, designed to prevent unauthorized plan switches by involving agents, consumers, and the Centers for Medicare & Medicaid Services (CMS). While this measure aimed to protect against fraudulent activity, it also slowed down legitimate plan changes, contributing to a decrease in overall switches.
Another factor contributing to the decline is the shift of states like Georgia from the federal marketplace to state-based exchanges. This transition removed approximately 300,000 enrollees from the federal enrollment count, further skewing the year-over-year comparisons.
Find Health Plans Online
Compare Plans By Carrier
The election year also played a role in impacting enrollment. The overlap of election season with the health insurance shopping period may have distracted potential enrollees, delaying their decision-making.
The Special Enrollment Period (SEP), which ran from April 2023 through 2024, provided individuals who lost Medicaid coverage the opportunity to enroll in ACA marketplace plans outside of the regular Open Enrollment Period (OEP). This shift had a notable effect on 2024 enrollment, as many new consumers turned to the marketplace for coverage.
Additional challenges arose from discrepancies between federal and state exchanges, ongoing premium increases, and concerns regarding the accuracy of last year’s enrollment data. A report from the Paragon Health Institute, a conservative think tank, claimed that up to 5 million Americans might be improperly receiving ACA subsidies. The report compared census data on potential subsidy eligibility with actual ACA enrollment numbers, suggesting that the subsidies may be over-distributed.
Compounding these issues, the CMS reported receiving around 90,000 complaints of unauthorized sign-ups or plan switches in the first quarter of 2024, adding to the uncertainty surrounding enrollment data.
These various factors illustrate the complexity of comparing ACA enrollment year over year. For health insurance professionals, understanding these dynamics and adapting strategies to address these challenges is crucial for navigating the evolving marketplace and effectively engaging consumers.


