Written by Erica Block
Reviewed by Garrett Ball
Expert Reviewer
We want to help you make educated healthcare decisions. While this post may have links to lead generation forms, this won’t influence our writing. We adhere to strict editorial standards to provide the most accurate and unbiased information.
All health insurance plans sold in the United States are required to set a maximum limit on the amount of money you have to spend on your own (or “out-of-pocket“) in a given year. This fixed-dollar amount is called an out-of-pocket maximum. Sometimes it’s called a “MOOP”, for maximum out-of-pocket.
By capping your out-of-pocket medical expenses, out-of-pocket maximums provide you with a level of financial protection in an emergency.
How Do Out-of-Pocket Maximums Work?
Once you spend enough money out-of-pocket on healthcare in a given year to reach your plan’s MOOP, your insurance provider will cover the full cost of any medical expenses you incur thereafter for the remainder of your insurance policy period. This usually lasts until the end of the calendar year.
Deductible VS. Out-of-Pocket Maximum
It’s common for people to confuse deductibles and MOOPs. While the terms are related, a deductible is the amount of money you have to pay out-of-pocket for covered healthcare services before your health insurance plan begins covering the cost for your care. An out-of-pocket limit helps you control a different kind of risk by placing a firm cap on the amount of money you’ll ever spend on healthcare in a given year.
Much like deductibles, your out-of-pocket maximum will reset at the end of your insurance policy period; neither the maximum, nor the amount you’ve spent toward it, will carry over from plan year to plan year.
In other words, after you meet your insurance deductible and spend enough in copayments and coinsurance to reach your MOOP, your health insurance provider will pay for any further healthcare you need, as long as you go to in-network doctors and receive care that is covered under the purview of your insurance plan.
Does Your Out-of-Pocket Maximum Include the Deductible?
Yes, your deductible is counted towards your out-of-pocket maximum. For example, let’s say you purchase an insurance plan with a $4,000 out-of-pocket maximum. If you fulfill your $1,000 deductible and spend $3,000 out-of-pocket in coinsurance fees by mid-year, any medical costs that you incur for the rest of the plan year will be 100 percent covered by your health insurance provider.
Which Healthcare Costs Count Toward Your Out-of-Pocket Maximum?
Policyholders can think of their out-of-pocket limit as their deductible + coinsurance + copayments up to a total dollar amount. Your premium, which you must continue paying to maintain your insurance coverage, doesn’t count toward your out-of-pocket limit.
Here is an overview of healthcare expenses which DO count toward your out-of-pocket maximum:
- Deductibles,
- Coinsurance fees,
- Copayments, and
- Any out-of-pocket healthcare expenditure for care and services qualifying as essential health benefits.
These healthcare expenses DO NOT count toward your out-of-pocket maximum limit:
- Monthly premiums;
- Balance billing charges for non-network providers;
- Out-of-network services. If you see a doctor who is not in-network, the cost of your visit cannot count toward your out-of-pocket maximum–even if your plan includes out-of-network coverage;
- Elective or cosmetic services. Elective procedures like cosmetic surgeries are not considered “medically necessary.” Read through your plan carefully to find out what’s covered by your insurer and what’s not;
- Any money spent on non-essential health benefits; and
- Adult dental or vision care, as most healthcare plans do not cover these services.
Some healthcare expenses may or may not count toward your out-of-pocket maximum, depending on the scope of your plan coverage. If you’re unsure whether an expense counts toward your annual out-of-pocket maximum, refer to your policy summary or call your insurance provider’s customer assistance line.
Out-of-Pocket Limits: Avoiding Confusion
Prior Authorization
Under some plans, certain healthcare services require prior authorization to count toward a policyholder’s out-of-pocket maximum. Your insurer may require your physician to authorize in advance a diagnostic test, such as blood tests, or imaging exams like MRIs or X-rays. If you don’t get authorization beforehand, your insurer may not cover the diagnostic exam, and charges for these services will not count toward your out-of-pocket limits
Essential Health Benefits
Out-of-pocket maximums only apply to covered essential health benefits. So if your plan doesn’t cover a particular treatment (i.e. acupuncture) or the service isn’t considered to be an essential benefit, it may not count toward your out-of-pocket maximum.
Confusion with Deductibles
Out-of-pocket limits are often confused with deductibles (the amount you pay out-of-pocket before coinsurance kicks in). Your deductible amount counts toward your out-of-pocket maximum and while copayments do count toward your out-of-pocket limit, they do not count toward your deductible.
MOOPs Under the Affordable Care Act
Under the Affordable Care Act (ACA), the federal government sets annual limits on the out-of-pocket spending maximums that apply to every healthcare plan sold in the United States. The government sets two different thresholds: there is an out-of-pocket maximum amount for individual healthcare plans and another out-of-pocket maximum amount for family healthcare plans covering two or more people. To keep pace with inflation, the Department of Health and Human Services increases OOP limits each year.
Out-of-Pocket Maximum: Individual VS Family
- For the 2020 plan year: The out-of-pocket limit for a Marketplace plan is $8,150 for an individual plan and $16,300 for a family plan (before any subsidies are applied).
- For the 2019 plan year: The out-of-pocket limit for a Marketplace plan was $7,900 for an individual plan and $15,800 for a family plan (before any subsidies are applied).
The ACA also stipulates that in addition to the family out-of-pocket limit, which (in 2019) cannot exceed $15,800, family plans are required to have an embedded individual out-of-pocket maximum, which applies to each family member covered under the same plan. In 2019, the “embedded” out-of-pocket limit cannot exceed $7,900 — the out-of-pocket maximum amount for individual coverage. In other words, individual out-of-pocket limits must be “embedded” in family health plans, such that a single member of a family cannot be required to pay more than $7,150.
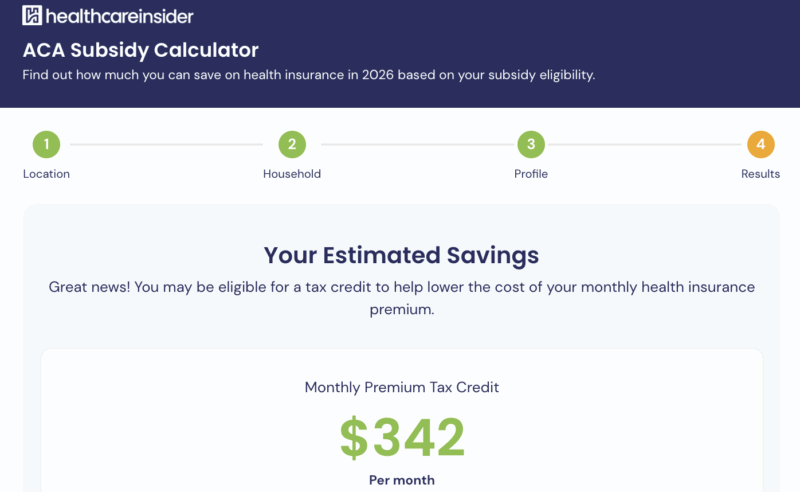
How the Subsidy for Your Out-Of-Pocket Maximum Works
The Affordable Care Act created health insurance subsidies to make health insurance more affordable for people with low-to-modest incomes. Whether you qualify for a cost-sharing subsidy – and the amount by which a subsidy will reduce your out-of-pocket limit – depends on your income. The closer your income is to the federal poverty level (FPL), the more your healthcare plan’s out-of-pocket maximum will be reduced.
Since both FPL and the federal limits on out-of-pocket maximum amounts change each year, the actual dollar amount of your subsidy is subject to change each year.
In order to benefit from a subsidy that reduces your out-of-pocket exposure, qualifying individuals must enroll in a “silver” plan through the federal, or one of the state Marketplaces.
If It’s a Subsidy, Do You Get Money?
The out-of-pocket maximum subsidy doesn’t literally give you money. Rather, the subsidy can potentially result in savings, since you will have to spend less money before reaching your plan’s out-of-pocket maximum.
Who Is Eligible for the Out-Of-Pocket Maximum Health Insurance Subsidy?
To qualify for a subsidy that reduces your out-of-pocket spending limit:
- Your income must be between 100-250 percent of the FPL;
- You must purchase your healthcare coverage through the federal Marketplace or your state’s health insurance exchange;
- You must select a “silver” tiered healthcare plan;
- If you’re married, you must file taxes jointly with your spouse. Filing separately will disqualify you (There’s a special exception for those who choose not to file jointly due to domestic abuse);
- You must reside in the United States legally;
- You cannot be incarcerated; and
- You cannot be eligible for ACA-compliant healthcare coverage through your employer.
Thank you for your feedback!


 by
Garrett Ball |
Updated on
February 20, 2026
by
Garrett Ball |
Updated on
February 20, 2026