Written by Adrienne Lin
We want to help you make educated healthcare decisions. While this post may have links to lead generation forms, this won’t influence our writing. We adhere to strict editorial standards to provide the most accurate and unbiased information.
Key Takeaways
-
Most Affordable Care Act (ACA) health plans are required to cover therapy and mental health services as essential health benefits.
-
Your costs depend on whether you use in-network vs. out-of-network providers, your deductible, and visit copays.
-
Short-term medical and limited-benefit plans don’t have to cover therapy, and many offer little or no mental health coverage.
-
Teletherapy is widely covered by insurers today, though cost-sharing may vary.
-
Always verify coverage before scheduling, as therapy benefits vary by plan, state, and provider type.
Overview
Mental health care has become a bigger priority than ever. With nearly 1 in 4 adults experiencing a mental illness in the U.S. each year, many people wonder: Does health insurance cover therapy, and how much will I actually pay?
The short answer—usually, yes, but the details depend on your plan, the provider, and the type of therapy you need. This guide breaks it all down in plain English so you can make informed decisions about your care.
How Health Insurance Covers Therapy
Health insurance coverage for therapy (also called outpatient mental health services) depends on federal rules, state mandates, and the type of plan you have. Here’s how it works.
ACA Plans Must Cover Mental Health Care
Under the ACA, and according to Healthcare.gov, marketplace and most employer plans must include mental health and substance use disorder services as one of the 10 essential health benefits. You can review the official government explanation on mental health and substance use coverage.
That means ACA-compliant plans usually cover:
-
Talk therapy (individual, group, family)
-
Cognitive behavioral therapy (CBT)
-
Medication management
-
Evaluations and screenings
-
Teletherapy
-
Substance use treatment
However, insurers can still set different cost-sharing levels, provider networks, and approval requirements. Coverage is not identical across plans.
Does Health Insurance Cover Different Types of Therapy?
Most Commonly Covered Therapy Types
| Therapy Type | Typically Covered? | Notes |
|---|---|---|
| Individual psychotherapy | Yes | Common benefit on ACA and employer plans |
| Family or couples therapy | Often | Coverage may depend on diagnosis |
| CBT, DBT, psychodynamic therapy | Yes | Must be medically necessary |
| Teletherapy / virtual visits | Yes on most plans | Cost-sharing varies |
| Substance use counseling | Yes | Required under mental health & SUD benefits |
| Group therapy | Yes | Often lower cost per session |
Sometimes or Partially Covered
-
EMDR (Eye Movement Desensitization and Reprocessing) – covered by many plans when medically necessary.
-
Marriage counselling is only sometimes covered, and insurers may require it to be tied to a diagnosed mental health condition.
-
If you’re wondering how health insurance handles married couples, check out our article on whether married couples can have separate health insurance.
-
Often Not Covered
Some plans exclude:
-
Life coaching
-
Career counselling
-
Hypnotherapy
-
Alternative treatments not recognized as evidence-based
Always confirm with your insurer before booking an appointment. Benefits vary significantly by plan.
How Much Does Therapy Cost With Insurance?
Costs depend on your plan’s deductible, copay, coinsurance, and whether the provider is in your network.
Typical Cost Ranges (varies by provider & plan)
-
In-network therapy: $10–$50 copay per visit, or 10–40% coinsurance after deductible
-
Out-of-network therapy: 50–80% of the session cost (if covered at all)
-
Teletherapy: Often the same cost-sharing as in-person visits
These amounts vary widely. Your insurer’s Summary of Benefits and Coverage (SBC) provides exact numbers.
A team of licensed insurance agents are here to help you compare plans
Does Insurance Cover Online Therapy?
Yes—most insurers now cover teletherapy, including video and sometimes phone sessions. Coverage expanded during COVID-19, and many insurers kept those benefits.
Things to check:
-
Whether your plan requires video vs. phone
-
If the telehealth platform is in-network
-
Whether session limits apply
-
If the provider must be licensed in your state
What Types of Insurance Plans Cover Therapy?
1. ACA Marketplace Plans
-
ACA plans must cover mental health services.
-
Must follow parity rules, meaning costs for mental health care cannot be more restrictive than for medical care. These rules, outlined by the Centers for Medicare & Medicaid Services (CMS), are detailed in the federal explanation of parity protections.
-
Usually cover teletherapy.
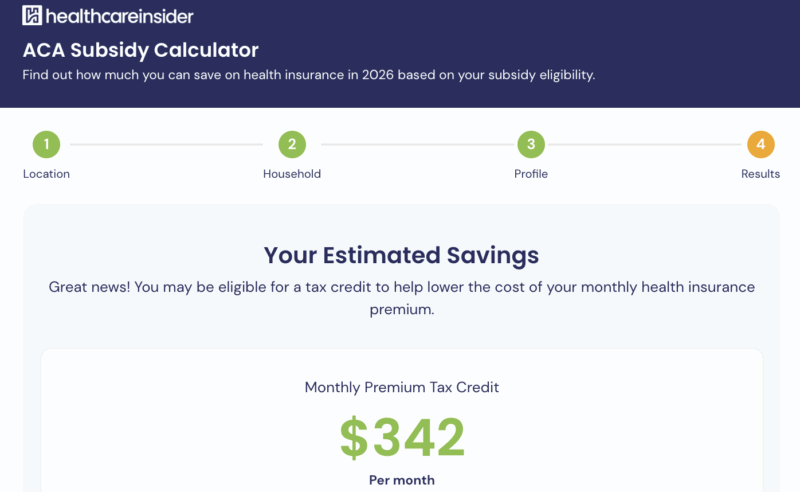
Use our updated ACA subsidy calculator to estimate your eligibilty to see if you can lower your monthly premiums.
2. Employer-Sponsored Insurance
Most employer plans cover therapy similarly to marketplace plans, but networks may be broader. Some employers also offer Employee Assistance Programs (EAPs) that provide a few no-cost therapy sessions.
3. Medicaid
Medicaid programs must cover mental health services for children under EPSDT rules and generally cover therapy for adults, though benefits vary by state. You can find state-level details on behavioral health services in Medicaid.
4. Medicare (Not the focus of this article, but worth noting)
Medicare covers therapy under Part B, but this article is focused on adults under age 65.
5. Short-Term Medical Plans
Short-term medical (STM) plans do not have to cover mental health benefits, and many don’t. Some cover only crisis-level care.
These plans are not required to follow ACA rules.
6. Fixed Indemnity or Supplemental Plans
These plans pay a flat amount per service and typically do not cover routine therapy visits. They are not major medical plans.
Learn more about ACA marketplace plans vs. private insurance plans to see what may fit your needs and budget.
How to Check Whether Your Insurance Covers Therapy
Here’s a simple step-by-step process.
1. Log in to your insurer account
Look for:
-
Mental health/behavioral health benefits
-
Copays or coinsurance
-
Deductible details
-
Telehealth coverage
2. Search the provider directory
Choose in-network therapists to keep costs lower.
3. Call the member services line
Ask:
-
-
“Is therapy covered on my plan?”
-
“What is my copay or coinsurance for mental health visits?”
-
“Do I need pre-authorization?”
-
“Is virtual therapy covered?”
-
“Are there session limits?”
-
4. Ask the therapist’s office
They can often check benefits for you.
Comparison: In-Network vs. Out-of-Network Therapy
| Therapy Type | Typically Covered? | Notes |
|---|---|---|
| Individual psychotherapy | Yes | Common benefit on ACA and employer plans |
| Family or couples therapy | Often | Coverage may depend on diagnosis |
| CBT, DBT, psychodynamic therapy | Yes | Must be medically necessary |
| Teletherapy / virtual visits | Yes on most plans | Cost-sharing varies |
| Substance use counseling | Yes | Required under mental health & SUD benefits |
| Group therapy | Yes | Often lower cost per session |
FAQs About Mental Health Coverage
Do you need a diagnosis for insurance to cover therapy?
Often, yes, most insurers require a medically necessary diagnosis (like anxiety or depression) for ongoing coverage. But initial evaluations are usually covered without one.
Does insurance cover couples therapy?
Sometimes, but often only if treatment is related to a mental health diagnosis. Coverage varies widely.
Is therapy covered before meeting my deductible?
If your plan charges a copay, you may pay only the copay.
If it uses coinsurance, you may pay full price until your deductible is met.
The Bottom Line
So, does health insurance cover therapy? In most cases, yes, especially if you’re enrolled in an ACA-compliant or employer-sponsored plan. But coverage amounts, provider networks, and costs differ widely, which is why it’s so important to check your specific benefits before booking an appointment.
If you’re ready to start therapy, your next steps should be:
-
Review your plan’s mental health benefits.
-
Choose a provider who accepts your insurance.
-
Ask about teletherapy options if you prefer virtual care.
-
Track your out-of-pocket costs to avoid surprises.
Prioritizing mental health is one of the best investments you can make in your overall well-being—and understanding your insurance coverage can make getting care much more affordable.
Thank you for your feedback!